Abstract. Background: Estrogen receptor beta (ERβ) belongs to a large family of nuclear receptors. Recent studies have suggested that ERβ in contrast to ERα might act as a tumour suppressor in ovarian cancer (OVCA). Materials and Methods:
Expression of ERβ was detected by immunocytochemistry in 11 OVCA cell lines and by immunohistochemistry in 43 (41 FIGO stage III) OVCA specimens prepared before chemotherapy and 30 specimens from the same group after chemotherapy.
Cisplatin sensitivity in the 11 cell lines was also analysed.
Results: No significant correlations between cisplatin- sensitivity and expression of ERβ was found in the cell lines.
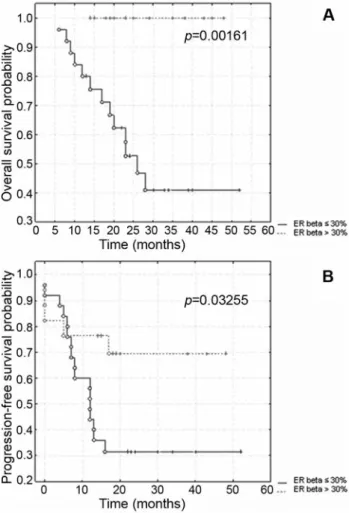
In the cases which responded well to chemotherapy (complete response) ERβ expression at preliminary laparotomy (PL) was significantly higher (p=0.0004) than in those with progressive disease. Kaplan-Meier analysis revealed that the patients with higher ERβ expression (>30% of cells) at PL had an increased overall survival time and progression-free time (p=0.00161 and p=0.03255, respectively) than the patients with lower ERβ espression. Significantly shorter overall survival time characterized the cases with lower immunoreactivity score of ERβ expression at secondary
cytoreduction (SCR) (p=0.00346). Conclusion: The loss of ERβ expression in ovarian tumours may be a feature of malignant transformation.
Ovarian cancer (OVCA) is one of the most lethal gynaecological carcinomas worldwide. About 190,000 new cases and 114,000 deaths from ovarian cancer are estimated to occur annually. The highest rates are reported in Scandinavia and Eastern Europe, the USA and Canada (1). Because early- stage OVCA (FIGO I or II) is generally asymptomatic, approximately 75% of women present with advanced disease at diagnosis which is associated with poor prognosis. Survival is highly dependent on the stage of the disease: 5-year survival in patients with early-stage is 80-90% compared to 25% for patients with advanced OVCA (2).
High serum levels of estrogen have been implicated as a risk factor for OVCA, but the cellular signal transduction pathways involved are not completely well known. The incessant ovulation hypothesis argues that trauma and repair of ovarian epithelium induced ovulation, contributes to OVCA development. Ovulatory cycles lead to long-term exposure of the epithelium to an estrogen-rich environment, which may promote cellular proliferation, including cyst formation and possibly malignant transformation (3).
Estrogen receptors, ER alpha (ERα) and ER beta (ERβ) belong to a large family of nuclear receptors and mediate the action of estrogens as ligand-dependent transcription factors (4). The molecular mechanisms of ERβ function in OVCA are still poorly established, but recent studies have suggested that ERβ in contrast to ERα might act as a tumour
Correspondence to: Agnieszka Halon, Department ofPathomorphology, Wroclaw Medical University, Marcinkowskiego 1, 50-368 Wroclaw, Poland. Tel: +48 717841240, Fax: +48 717840057, e-mail: ahalon2@gmail.com
Key Words: Estrogen receptor beta, ovarian cancer, prognostic factor, immunohistochemistry, cisplatin.
Loss of Estrogen Receptor Beta Expression Correlates with Shorter Overall Survival and Lack of Clinical Response
to Chemotherapy in Ovarian Cancer Patients
AGNIESZKA HALON
1, EWA NOWAK-MARKWITZ
2, ADAM MACIEJCZYK
3, MAREK PUDELKO
3, TSERENCHUNT GANSUKH
4, BALÁZS GYÖRFFY
5,6, PIOTR DONIZY
1, DAWID MURAWA
7, RAFAL MATKOWSKI
3,8, MAREK SPACZYNSKI
2, HERMANN LAGE
6and PAWEL SUROWIAK
3,6,9Departments of
1Pathomorphology,
8Oncology, and
9Histology and Embryology, Wroclaw Medical University, Wroclaw, Poland;
2
Department of Obstetrics and Gynaecology, University School of Medicine, Poznan, Poland;
3
Lower Silesian Oncology Centre, Wroclaw, Poland;
7
1st. Department of Surgical Oncology, Wielkopolska Cancer Center, Poznan, Poland;
4
Medical Research Institute of Mongolia, Bayangol duureg, Ulan Bator, Mongolia;
5
Semmelweis University Budapest, First. Department of Pediatrics, Budapest, Hungary;
6
Charité Campus Mitte, Institute of Pathology, Berlin, Germany
suppressor in OVCA (4, 5). Preliminary studies have revealed that ERβ levels, both protein and mRNA in OVCA decline relative to levels in the normal ovary (4, 6-8). Chan et al. (9), demonstrated that the immunoreactivity score of ERβ expression was significantly higher in normal tissue compared with malignant and its expression was a significant good predictor for disease-free survival and overall survival.
Furthermore, the absence of ERβ in OVCA might be a feature of malignant transformation (9).
From the 1970s, the ERs has evolved to be the most effective target for breast and ovarian cancer therapy.
Interactions between estradiol (E2) and ERs can be effectively blocked using a variety of agents, such as selective ER modulators (SERMs). Tamoxifen and raloxifen as a leading SERMs, are competitive inhibitors of E2 at the ERs and display distinct effects depending on the tissues (10). Only 15-18% of ER-positive OVCA initially respond to anti estrogen treatment based on blocking of estrogen-ER binding, in contrast to effective treatment of about 50% of ER-positive breast carcinomas (11). The most common mechanism of antiestrogen resistance is the absence of ER.
From the previous data, the role of tamoxifen in OVCA has not been properly established, although some authors have suggested that combined therapy with cisplatin and tamoxifen might reduced cisplatin resistance (12, 13).
The significance of ERβ expression in ovarian carcinogenesis and its impact on growth and survival of OVCA cells is still controversial. In this study, the expression of ERβ, in malignant epithelial ovarian tumours, and OVCA cell lines was investigated. Because cisplatin resistance is a major obstacle in the treatment of OVCA, analysis of cisplatin sensitivity in 11 OVCA cell lines was also performed.
Materials and Methods
Cell culture. The cisplatin-resistant cell line, A2780RCIS, was derived from the OVCA cell line, A2780 (14). The human OVCA cell lines CAOV-3, EFO 21, EFO 27, ES-2, Mdah 2774, OAW 42, OVCAR-3, PA-1 and SKOV-3 were kindly provided by Dr. Carsten Denkert (Institute of Pathology, Charité, Berlin, Germany). The human OVCA cells were grown in Leibovitz L-15 medium (Biowhittaker, Walkersville, MD, USA) supplemented with 10%
fetal calf serum (FCS) (GIBCO/BRL, Grand Island, NY, USA), 1 mM L-glutamine, 6.25 mg/l fetuin, 80 IE/l insulin, 2.5 mg/ml transferrin, 0.5 g/l glucose, 1.1 g/l NaHCO3, 1% minimal essential vitamins and 20,000 kIE/l trasylol in a humidified atmosphere of 5% CO2at 37˚C as described previously (14-17). In order to ensure maintenance of the cisplatin-resistant phenotype of the A2780RCIS cells, the medium was supplemented with 10 Ag/mL of cisplatin (33.3 μmol/L; GRY-Pharm, Kirchzarten, Germany).
Cell proliferation assay. Chemoresistance was tested using a proliferation assay based on sulphorhodamine B (SRB) staining as described previously (18). Briefly, 800 cells per well were seeded in 96-well plates in triplicate. After 24 h attachment, cisplatin was
added in dilution series for a 5-day incubation, before SRB staining was performed. Incubation with cisplatin was terminated by replacing the medium with 10% trichloroacetic acid, followed by incubation at 4˚C for 1 h. Subsequently, the plates were washed five times with water and stained by adding 100 μl 0.4% SRB (Sigma, St. Louis, MO,USA) in 1% acetic acid for 10 min at room temperature. Washing the plates five times with 1% acetic acid eliminated unbound dye. After air-drying and re-solubization of the protein bound dye in 10 mM Tris-HCl (pH=8.0) absorbance was read at 562 nm in an Elisa-Reader (EL 340 Microplate Bio Kinetics Reader, BIO-TEK Instruments, Winooski, VT, USA). The measurements were performed in triplicates in three independent experiments. The IC50-values were calculated from three independent experiments for each cell line.
Patients. Immunohistochemical examination was performed retrospectively on tissue samples taken for routine diagnostic purposes. Forty three patients who had undergone surgery in 1999- 2002 due to OVCA in the Department of Gynaecology and Obstetrics, University Medical School in Poznań, Poland were included in the study. The cases were selected based on availability of tissue and were not stratified for known preoperative or pathological prognostic factors. The study was approved by an Institutional Review Board (IRB) and the patients gave their informed consent before their inclusion into the study. Following the primary laparotomy (PL) all the patients were subjected to chemotherapy using cisplatin-based schemes (Table I). Thirty six patients from the same group were also subjected to secondary cytoreduction (SCR). In seven cases no second-look procedure was performed due to advancement of the disease. In six cases no tumour cells were detected in the material originating from the second-look procedure. The patients were monitored by periodic medical check- ups, ultrasonographic, radiological and cancer antigen 125 (CA-125) serum levels examinations. During the 52 months follow-up period, 22 patients (51%) had recurrent disease and 13 patients (30%) died of the disease. The mean progression-free survival time was 16.9 months (range 0 to 52 months), while the mean overall survival time was 24.6 months (range 6 to 52 months). Only the one stage I and one stage II patient achieved optimal cytoreduction.
Tissue samples were fixed in 10% buffered formalin and embedded in paraffin. In each case, hematoxylin and eosin stained preparations were subjected to histopathological evaluation by two pathologists.
The stage of the tumours was assessed according to the International Federation of Gynaecology and Obstetrics (19). Tumours were graded according to the Silverberg grading system (20).
Immunohistochemistry.Formalin-fixed, paraffin embedded tissue was freshly cut (4 μm). The sections were mounted on Superfrost slides (Menzel Gläser, Braunschweig, Germany), dewaxed with xylene and gradually hydrated. Activity of endogenous peroxidase was blocked by 5 min exposure to 3% H2O2. All the sections were boiled for 15 min at 250W in Antigen Retrieval Solution (DakoCytomation, Glostrup, Denmark). Then, immunohisto- chemical reactions were performed using the mouse mAb PPG5/10 (DakoCytomation) directed against ERβ 1 (dilution 1:50 in Antibody Diluent, Background Reducing (DakoCytomation) 1 h at 20˚C). Each reaction was accompanied by a negative control using Primary Mouse Negative Control (DakoCytomation). Subsequent incubations involved biotinylated antibodies (15 min, room temperature) and streptavidin-biotinylated peroxidase complex (15
min, room temperature) (Dako Detection System, LSAB+ and horseradish peroxidase, HRP, DakoCytomation). Diaminobenzidine (DAB, DakoCytomation) was used as a chromogen (7 min, at room temperature). All the sections were counterstained with Meyer’s hematoxylin. In this study, the Ki67 (21), and p53 (22) expression data, which had been investigated previously on the same group of patients (23), were reused.
Immunocytochemistry. Immunostaining of ERβ was performed in all the cell lines. The cells were grown on microscope slides and fixed in on ice-cold methanol-acetone mixture (1:1) for 10 min.
After re-hydration, the immunostaining reaction was performed in triplicate as described above. Furthermore, immunostaining of Ki67 was conducted for all the cell lines with mouse mAB against Ki67 (clone MIB-1; dilution 1:100 in Antibody Diluent, Background Reducing, DakoCytomation, 1 h at 20˚C).
Evaluation of reaction intensity. The intensity of the immunohistochemical and immunocytochemical reactions were estimated independently by two pathologists. Assessment of staining was “blinded” to sample details. In doubtful cases a re-evaluation was performed using a double-headed microscope and staining was discussed until a consensus was achieved. Immunostaining reactions
of p53 and Ki67 were evaluated using percentage of positive cells score. The expression of ERβ was graded using a semiquantitative scoring scale based on percentage of reactive cells (no staining=score 0, <10%=score 1, 10-30%=score 2, >30%=score 3).
Consequently, four possible products (0, 1, 2, 3) were obtained.
Statistical analysis. Statistical analysis of the results took advantage of Statistica 98 PL software (Statsoft, Krakow, Poland), SPSS software (release 10.0; SPSS Inc., Chicago, IL, USA) and Microsoft Office Excel 2007 (Microsoft Corporation, Redmond, WA, USA).
The employed tests included Mann-Whitney U-test, Spearman’s rank correlation, Chi-square and Kruskal-Wallis test. Kaplan-Meier statistics and log-rank tests were performed to estimate the significance of differences in survival times. The length of progression-free survival was defined as the time between the primary surgical treatment and diagnosis of a recurrent tumour or death.
Results
Cisplatin-sensitivity of cell lines. The sensitivity of the various human OVCA cell lines against treatment with cisplatin was determined by the assessment of IC
50values (Table II). The most sensitive cell line, PA-1, exhibited an IC
50of 0.75 μM, and the most cisplatin-resistant cell line, A2780RCIS, demonstrated an IC
50of 98.98 μM.
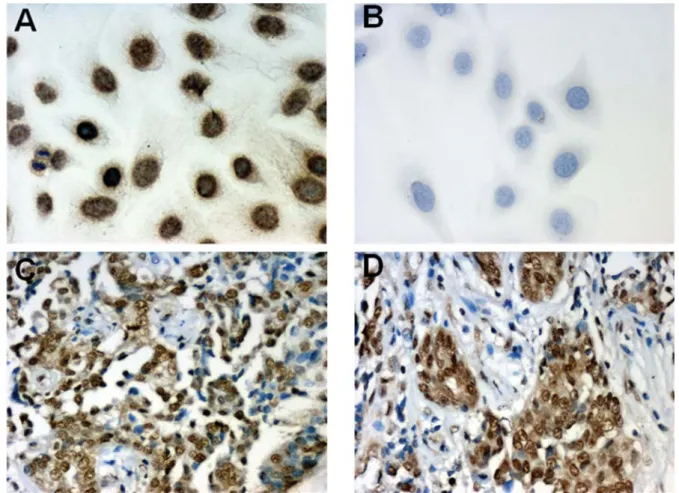
ERβ immunostaining in cell lines. Strong nuclear ERβ expression (score 3) was shown in the EFO 21 cells (Figure 1A). Interestingly, the immunocytochemical experiments showed that ERβ could also be detected in the cytoplasm of the OVCAR-3 and ES-2 cells (score 2 and 1, respectively).
The other cell lines were ERβ negative (Figure 1B, EFO 27 cells). No significant correlations were found between cisplatin-sensitivity and the expression of ERβ in the OVCA
Table I.Patient and tumour characteristics.Patient and tumour characteristics Nc %
All patients 43 100
Age (mean 51)a
≤50 20 47
50-60 16 37
>60 7 16
Gradea
1 7 16
2 18 42
3 18 42
FIGOa
I 1 2
II 1 2
III 41 95
Histologya
Serous 37 86
Endometrioid 3 7
Other 3 7
Clinical responseb
Complete response 16 37
Stable disease 5 12
Progressive disease 22 51
Chemotherapy (in total)
Cisplatin/Paclitaxel 31 72
Cisplatin/Cyclophosphamide/Adriblastin 6 14 Cisplatin/Cyclophosphamide/Paclitaxel 3 7 Cisplatin/Cyclophosphamide/Paclitaxel/Adriblastin 2 5
Carboplatin/Paclitaxel 1 2
aData are given for the first operation/diagnosis implemented.
bAccording to RECIST 1.0 (Response Evaluation Criteria in Solid Tumours) (29). cDifferences in the sum to 100 % in groups are due to rounding.
Table II. Chemosensitivity to cisplatin (IC50value) and immunoreactivity score of ERβ and Ki67 expression in human ovarian carcinoma cell lines.
Cell line ERβ ERβ Ki67 Cisplatin
expression expression expressiona IC50
nuclear cytoplasmic (μM)
A2780P 0 0 20 23.87
A2780RCIS 0 0 20 98.98
CAOV-3 0 0 60 1.92
EFO 21 3 0 10 5.08
EFO 27 0 0 15 2.25
ES-2 0 1 80 7.64
Mdah 2774 0 0 90 6.36
OAW 42 0 0 5 5.49
OVCAR-3 0 2 20 1.88
PA-1 0 0 80 0.75
SKOV-3 0 0 75 18.85
aPercentage of positive cells.
cell lines. Additionally, statistical analysis did not reveal any correlations between the expression of ERβ and Ki67.
Figures 2A and 2B present the expression of Ki67 in Mdah 2774 and OVCAR-3 cells, respectively.
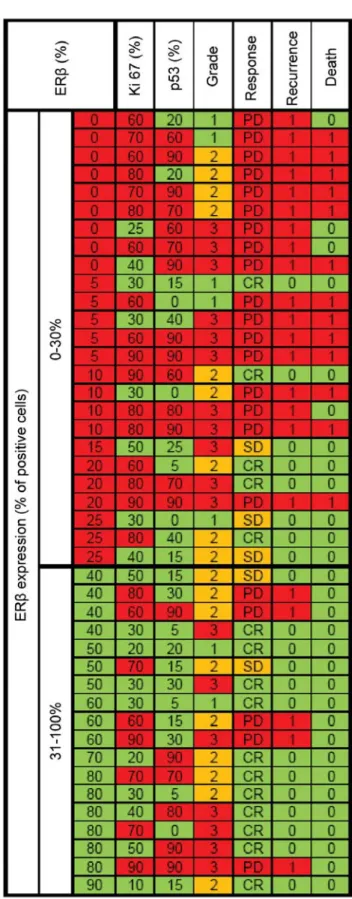
ERβ expression and clinicopathological and immunohisto- chemical parameters. Immunoreactivity of variable intensity was obtained in the individual OVCA cases (Figure 1C and D). At the first stage of statistical analysis of relationships between ERβ expression and clinicopathological parameters of the patients, the Kruskal-Wallis test was used. The relationship between the percentage of positive ERβ cells and the histological type of the tumour, the grade and the clinical response to chemotherapy was examined (Figure 3, Table III). In the cases which responded well to chemotherapy (complete response) based on cisplatin the immunoreactivity score of ERβ expression at PL was significantly higher (p=0.0004) than in patients with progressive disease (Figure 4). Statistical analysis did not reveal any significant correlations between ERβ expression and Ki67 and p53 percentage of positive cells (Table III).
In the Kaplan-Meier analysis overall survival time and progression-free time were compared between cases showing lower (0-30%) or higher (31-100% of positive cells) immunoreactivity score of ERβ expression at PL and SCR.
The patients with higher ERβ expression at PL had an increased overall survival time (Figure 5A) and an increased
Figure 1.Immunohistochemical localization of ERβ expression in EFO 21 cells (A., ×200; hematoxylin), EFO 27 cells (B., ×200; hematoxylin) and in ovarian cancer tissue (C., ×200, D., ×200; hematoxylin).Table III. Correlation between estrogen receptor beta expression and various clinicopathologic and immunohistochemical parameters.
Characteristics p-Value
Histological typea 0.6881
Gradea 0.5379
Clinical responsea 0.0004
Ageb 0.7932
Ki67b 0.2742
p53b 0.1647
CA-125b 0.7485
aANOVA rang Kruskal-Wallis. bSpearman’s rank correlation.
progression-free time (Figure 5B) than the patients with lower ERβ expression. The analysis also demonstrated that significantly shorter overall survival time characterized the cases with lower immunoreactivity score of ERβ expression at SCR (Figure 6A). No significant differences in progression-free time between the patients with lower and higher ERβ expression at SCR was observed (Figure 6B).
Since no significant relationships between the studied clinicopathological parameters (age, histology, grade, CA- 125 at PL level) and overall survival and progression-free time was found with univariate analysis (p>0.05), a multivariate analysis was not performed. Since 95% of the patients were in stage FIGO III, relationships between stage and survival data were not investigated.
Discussion
The most sensitive OVCA cell line, PA-1, exhibited an IC
50of 0.75 μM and the most cisplatin-resistant cell line, A2780RCIS, demonstrated an IC
50of 98.98 μM. However
Figure 2. Immunocytochemical localization of Ki67 expression in Mdah 2774 cells (A., ×200; hematoxylin) and OVCAR-3 cells (B., ×400; hematoxylin).Figure 3.Expression of ERβ at preliminary laparotomy in relation to clinical and pathological data of the patients. CR: complete response, SD: stable disease, PD: progressive disease.
Figure 4. Expression of ERβ and clinical response to chemotherapy.
Figure 5. Kaplan-Meier curves for survival in relation to ERβ expression at preliminary laparotomy.
Figure 6. Kaplan-Meier curves for survival in relation to ERβ expression at secondary cytoreduction.
no significant correlations between cisplatin-sensitivity and ERβ expression were found in the cell lines, nor were any correlations between expression of ERβ and Ki67 found.
Treeck et al. (24) studied the role of ERβ1 and two of its splice variants (ERβ-δ125, ERβ-δ1256) in the regulation of gene expression, apoptosis, cellular proliferation and migration of SKOV-3 OVCA cells and demonstrated that ERβ1 expression displayed multiple antitumoral effects.
The expression of ERβ in the tissue samples from OVCA patients was not correlated with the histopathological parameters, such as histological type and cancer grade. In the cases which responded well to chemotherapy based on cisplatin the immunoreactivity score of ERβ expression at PL was significantly higher (p=0.0004) than in the patients with progressive disease. Moreover, Kaplan-Meier analysis revealed that the patients with higher ERβ expression at PL had an increased overall survival time (p=0.00161) and an increased progression-free time (p=0.03255) than the patients with lower ERβ expression. Significantly shorter overall survival time also characterized the cases with lower of ERβ expression at SCR (p=0.00346).
The loss of ERβ expression in ovarian tumours may be a feature of malignant transformation. Chan et al. (9) in addition to showing that ERβ expression was significantly higher in normal ovary than malignant tissues, also showed significant correlations between the stage of disease and level of ERβ expression (higher in stage I than stage II-IV).
Multivariable analysis confirmed the role of ERβ in ovarian carcinogenesis, because its higher expression was found to be connected with longer disease-free survival as well as overall survival as confirmed in present study.
Several earlier studies have also investigated the status of ER status in relation to survival (25, 26). Interestingly, Fujimoto et al. (26) found that patients with a low or high ratio of ERα to ERβ had a significantly worse prognosis than patients with a more equal ratio.
In metastatic OVCA cells ERβ expression is often lost (27) however, its role in ovarian carcinogenesis is still unclear. EMT (epithelial-mesenchymal transition), a highly conserved process in which epithelial cells undergo a phenotypic switch to form mesenchymal-like cells, involves the loss of polarity and intracellular adhesion. These molecular and structural alterations are thought to allow dynamic cellular migration and the development of local and distant metastases. Park et al. identified ERβ overexpression as an important factor in the inhibition of prometastatic effects connected with the promotion of EMT in OVCA cells (28). Their results suggested that ERβ may have a function as a negative modulator of ERα in carcinogenesis of the ovary and the development of metastatic potential.
Overall, greater understanding of the role of ERβ expression in ovarian cancer may help to develop and
explore further the potential of hormonal therapy in ovarian tumours. Future studies on ERβ are needed to determine fully the clinicopathological implications of ERβ in ovarian carcinogenesis.
References
1 Colombo N, Van Gorp T, Parma G, Amant F, Gatta G, Sessa C and Vergote I: Ovarian cancer. Crit Rev Oncol Hematol 60: 159- 179, 2006.
2 Gatta G, Capocaccia R, De Angelis R, Stiller C, Coebergh JW the EUROCARE Working Group: Cancer survival in European adolescents and young adults. Eur J Cancer 39: 2600-2610, 2003.
3 Pearce ST and Jordan VC: The biological role of estrogen receptors α and β in cancer. Crit Rev Oncol Hem 50: 3-22, 2004.
4 Lazennec G: Estrogen receptor beta, a possible tumor suppressor involved in ovarian carcinogenesis. Cancer Letters 231: 151-157, 2006.
5 Cunat S, Hoffmann P and Pujol P: Estrogens and epithelial ovarian cancer. Gynecol Oncol 94: 25-32, 2004.
6 Bardin A, Hoffmann P, Boulle N, Katsaros D, Vignon F, Pujol P and Lazennec G: Involvement of estrogen receptor β in ovarian carcinogenesis. Cancer Res 64: 5861-5869, 2004.
7 Lindgren PR, Cajander S, Bäckström T, Gustafsson JA, Mäkelä S and Olofsson JI: Estrogen and progesterone receptors in ovarian epithelial tumors. Mol Cell End 221: 97-104, 2004.
8 Li AJ, Baldwin RL and Karlan BY: Estrogen and progesterone receptor subtype expression in normal and malignant ovarian epithelial cell cultures. Am J Obstet Gynecol 189: 22-27, 2003.
9 Chan KK, Wei N, Liu SS, Xiao-Yun L, Cheung AN and Ngan HY: Estrogen receptor subtypes in ovarian cancer. A clinical correlation. Obstet Gynecol 111: 144-151, 2008
10 Jordan VC, Gapstur S and Morrow M: Selective estrogen receptor modulation and reduction in risk of breast cancer, osteoporosis, and coronary heart disease. J Natl Cancer Inst 93:
1449-1457, 2001.
11 Kurebayashi J: Endocrine-resistant breast cancer: underlying mechanisms and strategies for overcoming resistance. Breast Cancer 10: 112-119, 2003.
12 Harries M and Kaye SB: Recent advances in the treatment of epithelial ovarian cancer. Expert Opin Investig Drugs 10: 1715- 1724, 2001.
13 McClay EF, Albright KD, Jones JA, Christen RD and Howell SB: Tamoxifen delays the development of resistance to cisplatin in human melanoma and ovarian cancer cell lines. Br J Cancer 70: 449-452, 1994.
14 Materna V, Liedert B, Thomale J and Lage H: Protection of platinum-DNA adduct formation and reversal of cisplatin resistance by anti-MRP2 hammerhead ribozymes in human cancer cells. Int J Cancer 115: 393-402, 2005.
15 Materna V, Stege A, Surowiak P, Priebsch A and Lage H: RNA interference-triggered reversal of ABCC2-dependent cisplatin resistance in human cancer cells. Biochem Biophys Res Commun 348: 153-157, 2006.
16 Kowalski P, Surowiak P and Lage H: Reversal of different drug- resistant phenotypes by an autocatalytic multitarget multiribozyme directed against the transcripts of the ABC transporters MDR1/P-gp, MRP2, and BCRP. Mol Ther 11: 508- 522, 2005.
17 Surowiak P, Materna V, Kaplenko I, Spaczynski M, Dolinska- Krajewska B, Gebarowska E, Dietel M, Zabel M and Lage H:
ABCC2 (MRP2, cMOAT) Can Be Localized in the Nuclear Membrane of Ovarian Carcinomas and Correlates with Resistance to Cisplatin and Clinical Outcome. Clin Cancer Res 12: 7149- 7158, 2006.
18 Györffy B, Surowiak P, Kiesslich O, Denkert C, Schäfer R, Dietel M and Lage H: Resistance prediction profile for eleven anticancer agents at clinical concentrations based on the gene expression pattern of thirty cell lines. Int J Cancer 118: 1699- 1712, 2006.
19 UICC TNM Classification of malignant tumors. Sobin LH, Wittekind Ch (eds). Wiley-Liss, New York, 1997.
20 Shimizu Y, Kamoi S, Amada S, Akiyama F and Silverberg SG:
Toward the development of a universal grading system of ovarian epithelial carcinoma: testing of a proposed system in a series of 461 patients with uniform treatment and follow-up.
Cancer 82: 893-901, 1998.
21 Surowiak P, Materna V, Kaplenko I, Spaczynski M, Dietel M, Lage H and Zabel M: Topoisomerase 1A, HER/2neu and Ki67 expression in paired primary and relapsed ovarian cancer tissue samples. Histol Histopathol 25: 131-139, 2006.
22 Materna V, Surowiak P, Markwitz E, Spaczynski M, Drag- Zalesinska M, Zabel M and Lage H: Expression of factors involved in regulation of DNA mismatch repair- and apoptosis pathways in ovarian cancer patients. Oncol Rep 17: 505-516, 2007.
23 Surowiak P, Materna V, Maciejczyk A, Kaplenko I, Spaczynski M, Dietel M, Lage H and Zabel M: CD46 expression is indicative of shorter revival-free survival for ovarian cancer patients. Anticancer Res 26(6C): 4943-4948, 2006.
24 Treeck O, Pfeiler G, Mitter D, Lattrich C, Piendl G and Ortmann O: Estrogen receptor β1 exerts antitumoral effects on SK-OV-3 ovarian cancer cells. J Endocrinol 193: 421-433, 2007.
25 Münstedt K, Steen J, Knauf AG, Buch T, von Georgi R and Franke FE: Steroid hormone receptors and long term survival in invasive ovarian cancer. Cancer 89: 1783-1791, 2000.
26 Fujimoto J, Hirose R, Sakaguchi H and Tamaya T: Clinical significance of expression of estrogen receptor alpha and beta mRNAs in ovarian cancers. Oncology 58: 334-341, 2000.
27 Rutherford T, Brown WD, Sapi E, Aschkenazi S, Muñoz A and Mor G: Absence of estrogen receptor-β expression in metastatic ovarian cancer. Obstet Gynecol 96: 417-421, 2000.
28 Park SH, Cheung LW, Wong AS and Leung PC: Estrogen regulates Snail and Slug in the down-regulation of E-cadherin and induces metastatic potential of ovarian cancer cells through estrogen receptor α. Mol Endocrinol 22: 2085-2098, 2008.
29 Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG; European Organization for Research and Treatment of Cancer: New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3): 205-216, 2000.