Teeth with Different MOD Cavity Dimensions
Andr ´as Forster, DMD ,1G ´abor Braunitzer, PhD,2M ´at ´e T ´oth, DMD,1Bal ´azs P. Szab ´o, PhD,3&
M ´ark Fr ´ater, DDS1
1Department of Operative and Esthetic Dentistry, Faculty of Dentistry, University of Szeged, Szeged, Hungary
2Department of Oral Surgery, Faculty of Dentistry University of Szeged, Szeged, Hungary
3Faculty of Engineering, Department of Food Engineering, University of Szeged, Szeged, Hungary
Keywords
Cavity dimensions; cusp coverage; maximal fracture strength; MOD cavity.
Correspondence
Andr ´as Forster, Faculty of Dentistry, University of Szeged, Tisza Lajos k ¨or ´ut 64.Szeged, H-6722, Hungary.
E-mail: andras.forster@me.com The authors deny any conflicts of interest related to this study.
Andr ´as Forster
http://orcid.org/0000-0002-3495-7105 Accepted November 30, 2017 doi: 10.1111/jopr.12777
Abstract
Purpose: Molar MOD (mesial-occlusal-distal) cavity preparation weakens relative cuspal stiffness by up to 63%, often resulting in cuspal fracture. This investigation inspects fracture resistance of MOD cavities restored using direct composite restora- tion.
Materials and Methods: 120 extracted, intact mandibular molars were selected.
MOD cavities with different depth/wall thickness were prepared in 9 groups (n= 12): A: 3 mm/3.5 mm, B: 3 mm/2.5 mm, C: 3 mm/1.5 mm, D: 5 mm/3.5 mm, E: 5 mm/2.5 mm, F: 5 mm/1.5 mm, G: 7 mm/3.5 mm, H: 7 mm/2.5 mm, I: 7 mm/1.5 mm.
Specimens with 7 mm deep cavities received root canal treatment. The teeth were restored with dental composite. Maximal fracture strength test was conducted. Intact natural teeth were used as control. For statistical analysis Kruskal-Wallis ANOVA with post-hoc pairwise comparisons was used (α=0.05).
Results: Significant difference was indicated between the control and groups D, E, F, G, H, and I. No significant differences were found between the A, B, C groups and the control. Comparing the 5 and 7 mm cavity depth groups, there was no statistical difference between any of them.
Conclusions: Within the limitations of this investigation, the following conclusions can be drawn regarding molar teeth with a MOD cavity: 3 mm or shallower cavities can be restored to the physiological fracture strength with direct composite restorations;
5 mm or deeper cavities cannot be restored to the physiological fracture strength with direct composite restorations. Cusp thickness does not significantly influence fracture strength in molar MOD cavities with a direct composite restoration.
Loss of tooth structure as a result of caries, trauma, or restora- tive and endodontic procedures has a negative influence on the fracture resistance of teeth and increases the risk of cusp fracture.1Studies have pointed out that the primary reason for tooth fragility in the posterior region is the presence of extensive cavity preparations2 and endodontic therapy.3 Endodontically treated posterior teeth present specific restorative challenges due to their more brittle behavior compared to vital teeth.4Ac- cording to Dietschi et al5this difference cannot be explained by their altered moisture content or dentine toughness, but rather the structural defect generated during tooth preparation; how- ever, according to several studies a conservative endodontic access cavity preparation in posterior teeth reduced the relative cuspal stiffness only by 5% to 20%.6,7Meanwhile a standard- ized MOD cavity preparation in maxillary premolar teeth was shown to result in an average loss of 63% in relative cuspal stiffness,8which is related principally to the loss of marginal
ridge integrity.9 This causes a reduction in fracture strength of approximately 54%.10,11 Complete cusp fracture of poste- rior teeth, especially with class II amalgam restorations, is a common phenomenon,12 highlighting the importance of the marginal ridges regarding the stability of the remaining oppos- ing walls. It seems that posterior cavities with intact marginal ridges are less susceptible to serious cusp deflection and re- sulting cuspal fracture than those with discontinued marginal ridges.
Depth and design of the cavity preparation have been shown to be the most critical factors for generating stress in enamel.13,14Cuspal deflection increases with increasing cavity dimensions,15meaning the larger the restoration’s volume, the higher the stress generated in the remaining dental structure.
Hood16reported that the remaining cusp after cavity prepara- tion acts as a cantilever beam under occlusal load. The floor of the cavity serves as a fulcrum for cusp bending, and the
Fracture Resistance of Adhesively Restored MOD Cavities Forsteret al
cantilever length increases with the depth of the cavity. Granath and Svensson17found that cusp displacement was directly re- lated to the extent of cavity width and depth. The width of the cavity correlates with the width of remaining cavity walls.
The residual cavity wall thickness represents the quantity of remaining enamel and dentin and is directly correlated with the residual sound tissue,1thus, measuring this parameter could be a simple but effective way to aid the selection of the appropriate type of future restoration.
Another important question in MOD (mesial-occlusal-distal) cavities both in vital and nonvital cases is the necessity of cuspal coverage. In endodontically treated teeth the provision of cuspal coverage is considered a key element in long-term success,18 since lowering of the remaining sound cusp to create cuspal coverage for protection of the intact cusp increased the fracture resistance.19 There is evidence to suggest that large prepara- tions require cuspal coverage to prevent possible fracture.20,21 Since the point at which onlays should be preferred over bonded inlays is a matter of debate,22this study aims to provide clini- cally useful and easily measurable information regarding cavity configuration and its prognosis on restorative decision making.
The question arises: What cavity depth and remaining wall thickness is restorable without cuspal coverage? The aim of this study is to assess the effect of different cavity configurations on the maximal fracture load strength of restored molar teeth, without cuspal coverage.
Materials and methods
All procedures of the study were approved by the local Ethics Committee, and the study was designed in accordance with the Declaration of Helsinki. One hundred and twenty mandibular third molars extracted for periodontal or orthodontic reasons were selected for this investigation. The freshly extracted teeth were immediately placed in 5.25% NaOCl for 5 minutes and then stored in 0.9% saline solution at room temperature until use, all within 2 months of extraction. During specimen prepa- ration, the soft tissue covering the root surface was removed with hand scalers. The inclusion criteria were visual absence of caries or root cracks, absence of previous endodontic treatment, posts or crown, or resorptions. Teeth with severe polymorphism of the coronal structures were excluded from the investigation.
Approximately 80% of the specimens ranged 10.0 to 10.9 mm in size, measured at the widest bucco-lingual di- mension, and the rest were between 11.0 and 12.0 mm. The mesio-distal dimension of the specimens was also measured, and this parameter allowed a maximum deviation of 10% from the determined mean. The height was between 8.0 and 9.0 mm measured from the cementoenamel-junction (CEJ). The 120 teeth were randomly distributed between 10 study groups (n= 12)3,18,22including 9 restored groups (Table 1) and a control group of intact natural teeth.
Cavity preparation
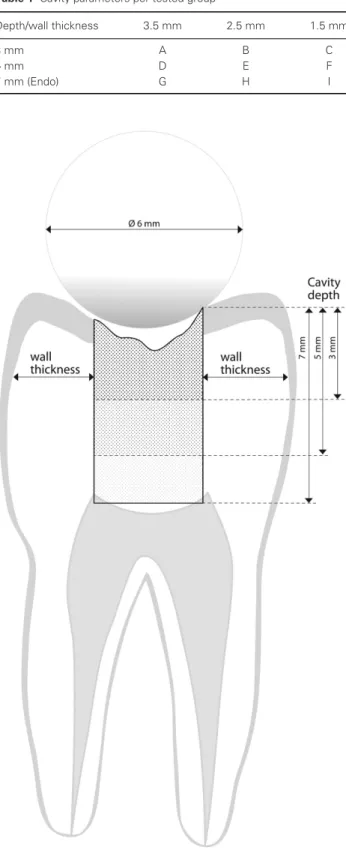
MOD cavities with different wall thicknesses and with different depths (Fig 1) were prepared by the same trained operator in 9 of the groups. The MOD cavities were prepared into each of the teeth according to the parameters listed in Table 1.
Table 1 Cavity parameters per tested group
Depth/wall thickness 3.5 mm 2.5 mm 1.5 mm
3 mm A B C
5 mm D E F
7 mm (Endo) G H I
Figure 1 Schematic orovestibular cross section of cavity proportions prepared in mandibular third molars subject to adhesive restoration and maximal fracture strength testing. Depth/wall thickness per group:
A: 3 mm/3.5 mm, B: 3 mm/2.5 mm, C: 3 mm/1.5 mm, D: 5 mm/3.5 mm, E: 5 mm/2.5 mm, F: 5 mm/1.5 mm, G: 7 mm/3.5 mm, H: 7 mm/2.5 mm, I: 7 mm/1.5 mm.
e326 Journal of Prosthodontics28(2019) e325–e331C2018 by the American College of Prosthodontists
The preparation was performed with a round-end parallel di- amond bur (881.31.014 FG; Brasseler USA Dental, Savannah, GA) initially positioned at the midline of the occlusal surface of the teeth (determined by dividing the distance between the buc- cal and lingual cusp tips by two). The thickness of the opposing walls at the cavity base was continuously checked during the preparation with a digital caliper (Mitutoyo Corp., Kawasaki, Japan). The cavity walls were prepared parallel to the axis of the tooth. The depth of the cavity was evaluated with a 15 UNC pe- riodontal probe (Hu-Friedy Mfg. Co., Chicago, IL) measured from the corresponding cusp tip by touching the cavity wall with the full length of the instrument. The cavity was one con- tinuous cavity with the proximal box having exactly the same width and depth as the occlusal one.
In the specimens in which the depth was meant to be 7 mm, an endodontic access was prepared, and endodontic treatment was carried out. After shaping with step-back technique (maximum file size 35-40), the root canals were filled with a thermoplasti- cized gutta percha delivery system (ObturaII; Obtura/Spartan, Fenton, MO). Following root canal obturation a base was ap- plied to the pulp chamber in the form of a 2.0- to 3.0-mm- thick resin modified glass-ionomer (Fuji II LC; GC Europe, Leuven, Belgium). barrier.23This was cut back with a coarse diamond bur (801.36.6801 FG/Surg; Brasseler USA Dental) to establish the 7 mm final depth of the cavity. The cavosurface margins were prepared perpendicular to the tooth surface. The cavity was rinsed with water and air-dried with an air/water syringe. After application of a Tofflemire (1101C 0.038; Kerr, Bioggio, Switzerland) matrix, the enamel was acid-etched se- lectively with 37% phosphoric acid for 15 seconds, rinsed with water, and air-dried. The cavity was adhesively treated with G-aenial Bond (GC Europe) according to the manufacturer’s instructions. The adhesive was light-cured for 40 seconds with an Optilux 501 halogen light (Kerr, Orange, CA) operating in standard mode at a light intensity of 740±36 mWcm2. In all groups, an approximately 0.5 mm-thin flow composite layer (G-aenial Flo A2; GC Europe) was applied on all walls of the cavity.24-26
This layer was light-cured for 40 seconds. After the flowable layer was applied, composite resin (Gradia Direct Anterior A2;
GC Europe) was placed in several consecutive 2 mm-thick oblique increments. Each increment was light cured from the occlusal surface for 40 seconds each, and after removal of the Tofflemire matrix band the mesial and distal sides were light cured for 20 seconds each (total 80 seconds). Light-curing times chosen were double that recommended by the manufacturer for each material used, in order to securely obtain maximal conversion at each layer.
The restorations were finished with a fine granular diamond bur (FG 7406-018, Jet Diamonds, Kerr, and FG 249-F012;
Horico, Berlin, Germany) and aluminum oxide polishers (One- Gloss PS Midi; Shofu Dental GmbH, Ratingen, Germany) and were stored in physiological saline solution (Isotonic Saline Solution 0.9%; B. Braun, Melsungen, Germany) in an incuba- tor (mco-18aic; Sanyo, Moriguchi, Japan) at 37°C. Specimens were subjected to a thermocycling process consisting of 500 cycles between hot- and cold-water baths of 5°and 55°C for 20 seconds each with an intermediate pause of 3 seconds’ trans- fer time in between.27
To simulate the periodontal ligament, the root surface of each tooth was coated with a layer of liquid latex separating material (Rubber-Sep; Kerr) prior to embedding. Specimens were em- bedded in methacrylate resin (Technovit 4004; Heraeus-Kulzer, Hanau, Germany) at 2 mm from the CEJ to simulate the bone level.
All specimens were tested for fracture strength within 24 hours of restoration, using a universal loading device (5848 MicroTester1; Instron, Norwood, MA), according to the method described by Wu et al.28Each test was performed at a 2 mm/min crosshead speed, and load was applied using a 6 mm diameter stainless-steel ball-shaped stylus positioned at the center of the occlusal surface of the tooth between the buccal and oral cusps in the central pit. A force vs. extension curve was dynamically plotted for each tooth. Fracture threshold—defined as the load at which the tooth-restoration complex exhibited the first frac- ture, resulting in a peak formation on the extension curve—was recorded in Newtons (N).
Statistical analysis was conducted in SPSS 21.0 (SPSS Inc., Chicago, IL). For the comparisons between the groups, Kruskal-Wallis ANOVA with post-hoc pairwise comparisons was used. The significance limit was set atα=0.05. The null hypothesis was that restored teeth are not weakened compared to the intact control specimens.
Results
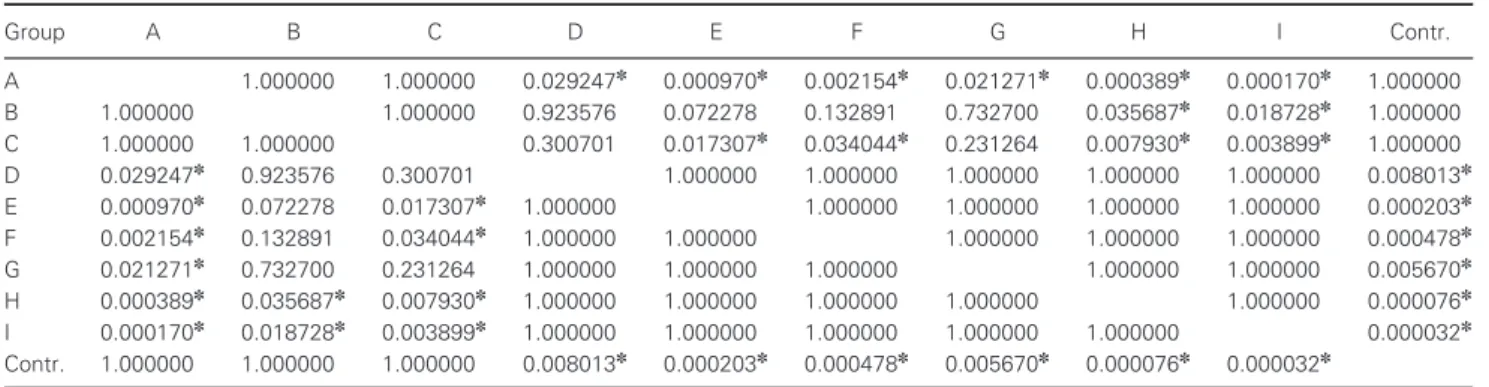
Median fracture strength values are presented in Figure 2. As the Kruskal-Wallis ANOVA indicated significant variance, post- hoc pairwise tests were performed. The pairwise tests indicated significant difference between the control group and all 5 and 7 mm groups (D, E, F, G, H, I). The 3 mm groups (A, B, C) did not show significant difference as compared to the control.
Significant difference was found between group A and all 5 and 7 mm groups (D, E, F, G, H, I). No significant differences were found between 3 mm cavity depth groups (A, B, C).
Comparing the 5 and 7 mm cavity depth groups, there was no statistical difference between any of them. The pairwise statistical analysis is detailed in Table 2. The null hypothesis was rejected, as the fracture strength of groups D, E, F, G, H, and I were significantly lower than that of the control group.
Discussion
A number of studies, with or without root canal preparation, have demonstrated that if the cavity involves the marginal ridge(s), the fracture resistance of the tooth is significantly reduced.28-30In this study the fracture resistance of MOD cav- ities varying from small through medium to large sizes was tested. These latter ones are considered to be typical of an amalgam replacement with the indication of an indirect or large direct restoration, which is becoming more common.30 The reason for the placement of large direct restorations is not only financial, but it is also a goal to preserve the tooth structure as much as possible, according to the principles of minimal in- tervention dentistry.32-35As found in previous studies, the depth of the preparation is one of the most critical factors in terms of future fracture.14,36In addition, the choice of the restorative method is commonly based on the cavity configuration and
Fracture Resistance of Adhesively Restored MOD Cavities Forsteret al
Figure 2 Mean fracture strength and standard deviation of the tested groups.
Table 2 Kruskal-Wallis ANOVA pairwise statistical analysis (p<0.00001). Significance indicated with✽symbol
Group A B C D E F G H I Contr.
A 1.000000 1.000000 0.029247✽ 0.000970✽ 0.002154✽ 0.021271✽ 0.000389✽ 0.000170✽ 1.000000
B 1.000000 1.000000 0.923576 0.072278 0.132891 0.732700 0.035687✽ 0.018728✽ 1.000000
C 1.000000 1.000000 0.300701 0.017307✽ 0.034044✽ 0.231264 0.007930✽ 0.003899✽ 1.000000
D 0.029247✽ 0.923576 0.300701 1.000000 1.000000 1.000000 1.000000 1.000000 0.008013✽
E 0.000970✽ 0.072278 0.017307✽ 1.000000 1.000000 1.000000 1.000000 1.000000 0.000203✽ F 0.002154✽ 0.132891 0.034044✽ 1.000000 1.000000 1.000000 1.000000 1.000000 0.000478✽
G 0.021271✽ 0.732700 0.231264 1.000000 1.000000 1.000000 1.000000 1.000000 0.005670✽
H 0.000389✽ 0.035687✽ 0.007930✽ 1.000000 1.000000 1.000000 1.000000 1.000000 0.000076✽ I 0.000170✽ 0.018728✽ 0.003899✽ 1.000000 1.000000 1.000000 1.000000 1.000000 0.000032✽ Contr. 1.000000 1.000000 1.000000 0.008013✽ 0.000203✽ 0.000478✽ 0.005670✽ 0.000076✽ 0.000032✽
dimensions and the number of residual cavity walls.37-39In this study the thickness of the cavity walls was measured with a den- tal caliper, and the depth was measured with a millimeter-scale periodontal probe.
Group A, having the most amount of dentine, showed the highest median fracture strength among the restored groups, whereas group I, having the largest cavity, thus the least amount of dentine, showed the lowest fracture resistance. This is in ac- cordance with previous research by Goel et al40and Torbj¨omer et al41 showing that preserving the anatomical structures and dentinal tissues is directly correlated with increased mechani- cal properties and less weakening of the tooth. The groups of 3 mm cavity depth (group A, B, C) presented the highest frac- ture resistance of all the restored specimens, and we found no significant difference in this respect between these three groups.
The 3 mm groups were also not significantly weaker compared to the control teeth. The relatively small cantilever beam from the occlusal margin to the cavity floor, is a possible explana-
tion for this finding. According to Hood’s hypothesis, cusps of teeth with MOD cavity preparations function as a cantilever beam, with the extent of deflection under load influenced by both beam thickness and length.16It seems from the results that when the cavity is shallow (3 mm deep), and thus the cantilever arm is small, the thickness of the walls is not a crucial factor in fracture strength.
When the cavity depth increased to 5 mm, but access cavity preparation was still not needed, the fracture strength dropped to approximately half of the value measured in group A. This could be caused by the increased depth leading to a greater can- tilever effect in these groups. With deeper cavity preparations the length of the freely deflectable cusp increases, and the cus- pal deflection increases.28,29 Jantarat et al42 found that cusps do not deform as simple cantilever beams, which seemingly contradicts the present findings.
In this study, cavity depth corresponding to an endodon- tic treatment (groups G, H, I) did not cause significant
e328 Journal of Prosthodontics28(2019) e325–e331C2018 by the American College of Prosthodontists
weakening, in comparison to the groups with 5 mm depth (groups D, E, F). This is in accordance with previous stud- ies conducted by Reeh et al, showing that when endodontic access is prepared after the preparation of a deep MOD cavity, the decrease measured in relative cuspal stiffness values is not significant compared to the values of MOD cavities without endodontic access.9,43
Based on the results of this investigation, 3 mm can be con- sidered a safe cavity depth for adhesive direct restorations. This is in accordance with Frater et al, who found that when restoring shallow MOD cavities with direct techniques using oblique lay- ering, there was no significant difference between the restored groups and the intact control group.45 These findings do not support the findings of Batalha-Silva et al,46 who concluded that 5 mm deep cavities could safely be restored with direct techniques. These results rather suggest that a cavity of 5 mm depth is already in the “danger zone” when talking about direct composite restorations without cusp coverage.
To aid clinical decision making, exact cavity dimensions or remaining tissue dimensions under which cuspal coverage must be provided would need to be established. As Seow et al found, maxillary premolars lost on average 53% of their stiffness when prepared with a MOD cavity with an isthmus width of one-third of the intercuspal distance, and if the isthmus width was half of the intercuspal distance, the prepared premolar teeth lost ap- proximately 67% of their stiffness.18 When a MOD cavity is loaded, force and stress is concentrated at the bottom corners of the prepared cavity.47Therefore, the thickness of the resid- ual cusp wall at the base could be a key element in decision making when it comes to preserving or eliminating cusps.48 According to Scotti et al37 and Deliperi et al,48 cavity walls with thickness greater than 2 mm should not be reduced, and cuspal coverage should be avoided, whereas “sufficient” thick- ness was defined as 2.5 mm in a later study by Scotti et al.49In this study reducing only the wall thickness, without changing the depth of the cavity, did not cause a significant reduction in fracture strength. From the results it seems that cavity wall thickness is only secondary to cavity depth in molar MOD cavities in terms of fracture strength, as the change in cavity wall thickness did not lead to a significant difference between the groups in the “safety zone” or between the “danger zone”
groups. Within the limitations of this study, this leads us to the conclusion that when the fracture safety of a cavity for a direct restoration without cusp coverage is to be determined, cavity depth is the primary determining factor. This is in accordance with the results of Morin et al50and Manhart et al,51who found that the depth of the preparation is the most critical factor in terms of future fractures. Since groups with cuspal coverage restorations were not included in this study, the results do not offer direct guidance on cuspal coverage. Also, since the cav- ities were only restored with a conventional adhesive direct composite restoration, the results cannot be extrapolated to sit- uations when fiber-reinforced materials are used; however, if the cavity depth of molar teeth with a MOD cavity reaches or exceeds 5 mm, cusp coverage with a direct or indirect adhe- sive restoration could be considered as a safety measure. Future investigations with similar methodology—involving cusp cov- erage with direct and indirect methods—need to be conducted to further our understanding on the effect of MOD cavity di-
mensions on the restorability of molar teeth and limitations of adhesive restorations.
According to Taha et al, “In experimental studies, fracture resistance to static loading has been used as a measure of the effect of cavity preparation and/or restoration on tooth strength.
Although the fracture load is typically much higher than func- tional occlusal loads, it is still a valid method for comparing restorative materials and different cavity designs.”52The use of a 6 mm steel sphere for resistance to fracture testing by Dietschi et al53 and Soares et al54 was shown to be ideal for molars, because it contacts the functional and nonfunctional cusps in positions close to those found clinically. Also, in the current study, the teeth were subjected to vertical compressive loading with a stainless steel sphere 6 mm in diameter.
Conclusions
Within the limitations of this investigation, the following con- clusions can be drawn:
1. Molar teeth with 3 mm or shallower depth MOD cavities can be restored to the same fracture resistance as intact teeth with a direct composite restoration, regardless of cavity wall thickness.
2. Molar teeth with 5 mm or higher depth MOD cavities cannot be restored to the physiological fracture resistance with a direct composite restoration, regardless of cavity wall thickness.
3. Cusp thickness does not significantly influence frac- ture strength in MOD cavities with a direct composite restoration.
Acknowledgments
The authors wish to thank Dean Kinga Turz´o and Prof. Katalin Nagy for their support in realizing the project. We also express our gratitude to Prof. Dr. Gyula S´ary for his valuable contribu- tion to the statistical analysis.
References
1. ElAyouti A, Serry MI, Geis-Gerstorfer J, et al: Influence of cusp coverage on the fracture resistance of premolars with endodontic access cavities. Int Endod J 2011;44:543-549
2. Larson TD, Douglas WH, Geistfeld RE: Effect of prepared cavities on the strength of teeth. Oper Dent 1981;6:2-5 3. Soares PV, Santos-Filho PC, Martins LR, et al: Influence of
restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part I: fracture resistance and fracture mode. J Prosthet Dent 2008;99:30-37 4. Magne P, Knezevic A: Thickness of CAD-CAM composite resin
overlays influences fatigue resistance of endodontically treated premolars. Dent Mater 2009;25:1264-1268
5. Dietschi D, Duc O, Krejci I, et al: Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature—Part 1. Composition and micro- and macrostructure alterations. Quintessence Int 2007;38:733-743 6. Rocca GT, Krejci I: Crown and post-free adhesive restorations
for endodontically treated posterior teeth: from direct composite to endocrowns. Eur J Esthet Dent 2013;8:156-179
7. Tay FR, Pashley DH: Monoblocks in root canals: a hypothetical or a tangible goal. J Endod 2007;33:391-398
Fracture Resistance of Adhesively Restored MOD Cavities Forsteret al
8. El-Helali R, Dowling AH, McGinley EL, et al: Influence of resin-based composite restoration technique and endodontic access on cuspal deflection and cervical microleakage scores. J Dent 2013;41:216-222
9. Reeh ES, Douglas WH, Messer HH: Stiffness of
endodontically-treated teeth related to restoration technique. J Dent Res 1989;68:1540-1544
10. Hannig C, Westphal C, Becker K, et al: Fracture resistance of endodontically treated maxillary premolars restored with CAD/CAM ceramic inlays. J Prosthet Dent 2005;94:342-349 11. Seo DG, Yi YA, Shin SJ, et al: Analysis of factors associated
with cracked teeth. J Endod 2012;38:288-292
12. Fennis WM, Tezvergil A, Kuijs RH, et al: In vitro fracture resistance of fiber reinforced cusp-replacing composite restorations. Dent Mater 2005;21:565-572
13. Hansen EK, Asmussen E: In vivo fractures of endodontically treated posterior teeth restored with enamel-bonded resin. Endod Dent Traumatol 1990;6:218-225
14. Lin CL, Chang CH, Ko CC: Multifactorial analysis of an MOD restored human premolar using auto-mesh finite element approach. J Oral Rehabil 2001;28:576-585
15. Taha NA, Palamara JE, Messer HH: Cuspal deflection, strain and microleakage of endodontically treated premolar teeth restored with direct resin composites. J Dent 2009;37:724-730 16. Hood JA: Biomechanics of the intact, prepared and restored
tooth: some clinical implications. Int Dent J 1991;41:25-32 17. Granath L, Svensson A: Elastic outward bending of loaded
buccal and lingual premolar walls in relation to cavity size and form. Scand J Dent Res 1991;99:1-7
18. Seow LL, Toh CH, Wilson NH: Strain measurements and fracture resistance of endodontically treated premolars restored with all-ceramic restorations. J Dent 2015;43:126-132 19. Fennis WM, Kuijs RH, Kreulen CM, et al: Fatigue resistance of
teeth restored with cuspal-coverage composite restorations. Int J Prosthodont 2004;17:313-317
20. Burke FJ: Tooth fracture in vivo and in vitro. J Dent 1992;20:131-139
21. Burke FJ, Wilson NH, Watts DC: The effect of cavity wall taper on fracture resistance of teeth restored with resin composite inlays. Oper Dent 1993;18:230-236
22. St-Georges AJ, Sturdevant JR, Swift Jr EJ, et al: Fracture resistance of prepared teeth restored with bonded inlay restorations. J Prosthet Dent 2003;89:551-557
23. Magne P, Carvalho AO, Bruzi G, et al: Influence of no-ferrule and no-post buildup design on the fatigue resistance of endodontically treated molars restored with resin nanoceramic CAD/CAM crowns. Oper Dent 2014;39:595-602
24. Jayasooriya PR, Pereira PN, Nikaido T, et al: Efficacy of a resin coating on bond strengths of resin cement to dentin. J Aesthet Restor Dent 2003;15:105–113
25. Tay FR, Pashley DH: Have dentin adhesives become too hydrophilic? J Can Dent Assoc 2003;69:726-731
26. Pongprueksa P, Kuphasuk W, Senawongse P: Effect of elastic cavity wall and occlusal loading on microleakage and dentin bond strength. Oper Dent 2007;32:466-475
27. Kivanc BH, Alacam T, Gorgul G: Fracture resistance of premolars with one remaining cavity wall restored using different techniques. Dent Mater J 2010;29:262-267
28. Wu Y, Cathro P, Marino V: Fracture resistance and pattern of the upper premolars with obturated canals and restored endodontic occlusal access cavities. J Biomed Res 2010;24:474-478 29. Lee MR, Cho BH, Son HH, et al: Influence of cavity dimension
and restoration methods on the cusp deflection of premolars in composite restoration. Dent Mater 2007;23:288-295
30. Meredith N, Setchell DJ: In vitro measurement of cuspal strain and displacement in composite restored teeth. J Dent
1997;25:331-337
31. Cara RR, Fleming GJ, Palin WM, et al: Cuspal deflection and microleakage in premolar teeth restored with resin-based composites with and without an intermediary flowable layer. J Dent 2007;35:482-489
32. Mount GJ, Ngo H: Minimal intervention: a new concept for operative dentistry. Quintessence Int 2000;31:527-533 33. Yamada Y, Tsubota Y, Fukushima S: Effect of restoration
method on fracture resistance of endodontically treated maxillary premolars. Int J Prosthodont 2004;17:94-98
34. Cobankara FK, Unlu N, Cetin AR, et al: The effect of different restoration techniques on the fracture resistance of
endodontically-treated molars. Oper Dent 2008;33:526- 533
35. Assif D, Gorfil C: Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent 1994;71:565- 567
36. Khers SC, Carpenter CW, Vetter JD, et al: Anatomy of cusps of posterior teeth and their fracture potential. J Prosthet Dent 1990;64:139-147
37. Scotti N, Rota R, Scansetti M, et al: Influence of adhesive techniques on fracture resistance of endodontically treated premolars with various residual wall thicknesses. J Prosthet Dent 2013;110:376-382
38. Nam SH, Chang HS, Min KS, et al: Effect of the number of residual walls on fracture resistances, failure patterns, and photoelasticity of simulated premolars restored with or without fiber-reinforced composite posts. J Endod 2010;36:297-301 39. Mangold JT, Kern M: Influence of glass-fiber posts on the
fracture resistance and failure pattern of endodontically treated premolars with varying substance loss: an in vitro study. J Prosthet Dent 2011;105:387-393
40. Goel VK, Khera SC, Gurusami S, et al: Effect of cavity depth on stresses in a restored tooth. J Prosthet Dent 1992;67:174-183 41. Torbjorner A, Fransson B: Biomechanical aspects of prosthetic
treatment of structurally compromised teeth. Int J Prosthodont 2004;17:135-141
42. Jantarat J, Panitvisai P, Palamara JE, et al: Comparison of methods for measuring cuspal deformation in teeth. J Dent 2001;29:75-82
43. Reeh ES, Messer HH, Douglas WH: Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod 1989;15:512-516
44. Eakle WS, Maxwell EH, Braly BV: Fractures of posterior teeth in adults. J Am Dent Assoc 1986;112:215-218
45. Frater M, Forster A, Kereszturi M, et al: In vitro fracture resistance of molar teeth restored with a short fibre-reinforced composite material. J Dent 2014;42:1143-1150
46. Batalha-Silva S, de Andrada MA, Maia HP, et al: Fatigue resistance and crack propensity of large MOD composite resin restorations: direct versus CAD/CAM inlays. Dent Mater 2013;29:324-331
47. Bell JG, Smith MC, de Pont JJ: Cuspal failures of MOD restored teeth. Aust Dent J 1982;27:283-287
48. Deliperi S, Bardwell DN: Multiple cuspal-coverage direct composite restorations: functional and esthetic guidelines. J Esthet Restor Dent 2008;20:300-312
49. Scotti N, Eruli C, Comba A, et al: Longevity of class 2 direct restorations in root-filled teeth: a retrospective clinical study. J Dent 2015;43:499-505
50. Morin D, DeLong R, Douglas WH: Cusp reinforcement by the acid-etch technique. J Dent Res 1984;63:1075-1078
e330 Journal of Prosthodontics28(2019) e325–e331C2018 by the American College of Prosthodontists
51. Manhart J, Kunzelmann KH, Chen HY, et al: Mechanical properties and wear behavior of light-cured packable composite resins. Dent Mater 2000;16:33-40
52. Taha NA, Palamara JE, Messer HH: Fracture strength and fracture patterns of root filled teeth restored with direct resin restorations. J Dent 2011;39:527-535
53. Dietschi D, Maeder M, Meyer JM, et al: In vitro resistance to fracture of porcelain inlays bonded to tooth. Quintessence Int 1990;21:823-831
54. Soares CJ, Martins LR, Pfeifer JM, et al: Fracture resistance of teeth restored with indirect-composite and ceramic inlay systems.
Quintessence Int 2004;35:281-286