IIVS#1538397, VOL 0, ISS 0
Reconstruction of Alar-Perialar Defects with a Combined Subcutaneous and Cutaneous Pedicled Rotation-Advancement Nasolabial Flap
Gabor Mohos,Ad am Kocsis, Gabor Er}os, Csilla Korponyai,Akos Varga, Bal azs Bende, and Janos Varga
QUERY SHEET
This page lists questions we have about your paper. The numbers displayed at left can be found in the text of the paper for reference. In addition, please review your paper as a whole for correctness.
Q1. Please provide the volume number for Ref. [6].
TABLE OF CONTENTS LISTING
The table of contents for the journal will list your paper exactly as it appears below:
Reconstruction of Alar-Perialar Defects with a Combined Subcutaneous and Cutaneous Pedicled Rotation-Advancement Nasolabial Flap
Gabor Mohos, Ad am Kocsis, Gabor Eros, Csilla Korponyai,} Akos Varga, Bal azs Bende, and Janos Varga
Reconstruction of Alar-Perialar Defects with a Combined Subcutaneous and Cutaneous Pedicled Rotation-Advancement Nasolabial Flap
Gabor Mohos, Ad am Kocsis, Gabor Er}os, Csilla Korponyai, Akos Varga, Bal azs Bende, Janos Varga
Department of Dermatology and Allergology, University of Szeged, Szeged, Hungary
ABSTRACT
Aim of the Study: During the reconstruction of alar defects involving the upper lip, reconstructive surgeons face the need for various thicknesses of tissues crucial to preserving the facial sulcus which is important for a cosmetically acceptable result. Our aim was to reconstruct the deep perialar and thinner lateral nasal alar defect in a single step procedure with a suitable flap which is reliable, has appropriate blood supply and provides an esthetically good result.Materials and Methods: Extended alar defect was reconstructed with a combined flap in 10 cases. During the procedure, a subcutaneous pedicle was created and the proximal part of the flap was rotated into the defect as a rotational flap. The procedure and the follow-up have been photo-documented in all cases. Furthermore, the perfusion of the flaps was monitored by means of laser Doppler flowmetry. Postoperative complications were evaluated with a semi-quantitative score and the patients completed a patient satisfaction questionnaire, too.Results: An optimal esthetic result was obtained in all cases after the operation. The lateral nasal alar part of the defect was reconstructed with the thinner proximal part of the flap while the deeper perialar region involving the upper lip was covered with the thicker distal part. The flaps have shown sufficient blood flow after the operation. There was no significant pin cushioning or “trap-door” effect in any case. Mild erythema and edema was found in few cases. The patients were satisfied with the cosmetic result of the intervention.Conclusions: The flap is suitable for the reconstruction of alar defects involving the perialar region. It has the advantage of covering the deeper peri- alar and the thinner alar defects, whilst eliminating the pin cushioning effect of the conventional subcutane- ous island pedicle flaps.
Keywords: cutaneous pedicle flap; subcutaneous pedicle flap; skin defect; combined flap; perialar reconstruction
INTRODUCTION
Skin malignancies often develop on the lateral nasal alar and adjacent regions [1]. According to a recent study, 33% of nasal skin tumors affect the alar area [2].
The remaining defect usually involves multiple cos- metic units, destroying the supra-alar, alar-facial groove, and the melolabial fold [1]. Traditionally, the defined C- shaped perialar area includes the superior labial tissue, melolabial fold, medial cheek, and nasal tissue superior to the nasal alar crease [3].
If the defect is localized to a single esthetic unit and side-to-side closure is not possible, owing to the size, V-Y advancement island pedicle flap is the most frequently chosen technique [4]. It is an important principle that if the defect affects more than 50% of an esthetic subunit, the whole subunit is advised to be reconstructed with the excision of the remaining subunit [2]. Maintenance of the nat- ural curvatures and facial symmetry without impaired airflow are important factors when per- forming flap closure in the alar region [2]. Defects 1
2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56
57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112
Received 10 July 2018; accepted 16 October 2018.
Gabor Mohos andAd am Kocsis contributed equally to the work.
Address correspondence to Gabor Er}os, Department of Dermatology and Allergology, University of Szeged, Koranyi fasor 6., 6720 Szeged, Hungary. E-mail:eros.gabor@med.u-szeged.hu
localized to the nasal ala and C-shaped region usu- ally require multiple combined flaps and further additional procedures (e.g. pedicle plasty in case of interpolational flap or correctional procedures to obtain optimal esthetic result). The present study introduces a variation of cutaneous-subcutaneous pedicled rotation-advancement flap for the recon- struction of the thin alar and adjacent deep perialar defects in a single step procedure with an appropri- ate cosmetic result.
MATERIALS AND METHODS Patients
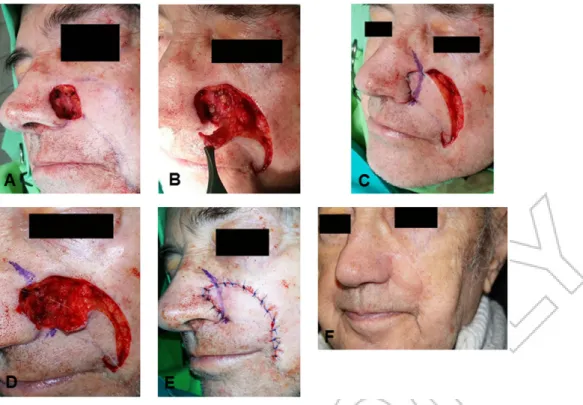
Ten patients were included in this study, mean age was 77 years (ranges from 66 to 84 years, 6 males, 4 females). Skin defect was localized to the alar region, the alar-facial groove, the upper lip and the cranial part of the nasolabial fold after the tumor was removed (Figure 1A). The extent of the defects following tumor excision ranged from 1.8 cm 1.8 cm to 2.62.9 cm. Histological examination revealed basal cell carcinoma with tumor-free mar- gins in all cases. Reconstruction was only performed once final histological result was obtained. This took 2–3 days, during which period a temporary coverage was used (Epigard, Biovision GmbH, Ilmenau, Germany). The mean follow-up was 7.5 months
(ranges from 5 to 15 months). Prior to the interven- tion, all participants have given their informed con- sent in writing which granted the authors to use their photographs for scientific purpose.
Surgical Procedures
Both the removal of the tumor and the reconstruc- tion were performed under local anesthesia. The flap was designed by marking the nasolabial fold and a curved line from the distal-lateral part of the defect according to the relaxed skin tension lines.
These lines matched in a distal point, marking the size and shape of the flap. Incision was performed on the lateral line, followed by subcutaneous tissue dissection and mobilization of the lateral wound edge, if necessary. It is important not to undermine the flap during the preparation and mobilization of the pedicle and to keep the perforator branches of the facial artery intact to preserve the vascular sup- ply of the flap (Figure 1B). The cutaneous branches from the medial part and the subcutaneous perfor- ator branches from the inferior part of the flap were hereby preserved. The flap was pulled to the cranial point of the defect. If necessary, a cut back was per- formed distally in the nasolabial fold so that the flap could be easily placed into the defect. Following temporary fixation of the proximal part a marking was performed on the flap according to the alar- 113
114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 150 151 152 153 154 155 156 157 158 159 160 161 162 163 164 165 166 167 168 169 170
171 172 173 174 175 176 177 178 179 180 181 182 183 184 185 186 187 188 189 190 191 192 193 194 195 196 197 198 199 200 201 202 203 204 205 206 207 208 209 210 211 212 213 214 215 216 217 218 219 220 221 222 223 224 225 226 227 228
FIGURE 1 Different steps of the operation. A: preoperative status, B: dissection of the subcutaneous and cutaneous pedicled flap, C: temporarily situated flap, blue ink shows the position of alar-facial groove on the skin flap, D: alar-facial groove is fixed with 5/0 absorbable sutures, E: the flap is sutured into the defect, F: late postoperative status.
2 G. Mohoset al.
Journal of Investigative Surgery
facial groove (Figure 1C). The flap was thinned proximally from this marking. This part was used to cover the alar fragment of the defect. The prospect- ive fold can be fixed to its base in the alar-facial groove with one or two 5/0 absorbable sutures if the flap is elevated (Figure 1D). Wound closure was performed with 5/0 absorbable and 5/0 permanent sutures (Figure 1E). Drainage or compression was not necessary. Scars were treated with silicone-oint- ment. Massage of the flap was advised after 4 weeks postoperatively (Figure 1F).Figures 2–4demonstrate the steps of operation in three other patients.
Patients were discharged on 2nd–3rd postopera- tive day. An examination was performed 10 days after the surgery, stitches were removed this time.
The second examination was in the 3rd postopera- tive week. Following this, the patients were exam- ined in each 3 months. During the postoperative period, different complications were monitored and evaluated as described below. If it was necessary, antibiotic therapy was launched which involved daily 1,000 mg cefuroxime (2500 mg) adminis- tered orally.
Laser Doppler Flowmetry
Laser Doppler flowmetry was chosen for the deter- mination of the microcirculation since it is an accepted and reliable method for this aim [5].
Perfusion of the flaps was monitored by means of
the PeriFlux System 5000 (Perimed, J€arf€alla, Sweden), as described in a previous study [6]. The sensor was fixed to the tissue with a sterile adhesive strip pro- vided by the manufacturer. Measurements were per- formed at five different time points: before the incision (baseline), after preparation of the flap, after fixation of the flap, 1 day after surgery and 3 weeks after surgery. At each time point, recordings were made for 5 minutes. Perisoft for Windows software was used for data collection, storage and analysis.
The data are presented as perfusion unit (P.U.).
Evaluation of Complications
The following signs and aspects were monitored:
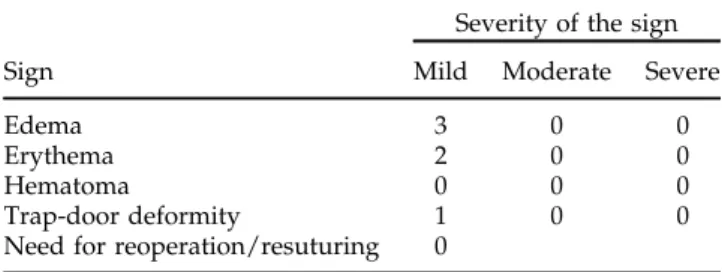
edema, erythema, hematoma, trap-door deformity and need for resuturing/reoperation (Table 1).
Complications were evaluated with a semi quantita- tive scoring system. Briefly, 0: the given sign is not present; 1, 2, 3: mild, moderate, and severe manifest- ation of the given sign, respectively.
Patient Satisfaction
Each patient was asked to complete a patient satis- faction questionnaire in the 6th postoperative month. Eight questions were given concerning the postoperative pain and the satisfaction with the results of the intervention (Table 2). Patients were 230
231 232 233 234 235 236 237 238 239 240 241 242 243 244 245 246 247 248 249 250 251 252 253 254 255 256 257 258 259 260 261 262 263 264 265 266 267 268 269 270 271 272 273 274 275 276 277 278 279 280 281 282 283 284 285 286
288 289 290 291 292 293 294 295 296 297 298 299 300 301 302 303 304 305 306 307 308 309 310 311 312 313 314 315 316 317 318 319 320 321 322 323 324 325 326 327 328 329 330 331 332 333 334 335 336 337 338 339 340 341 342 343 344
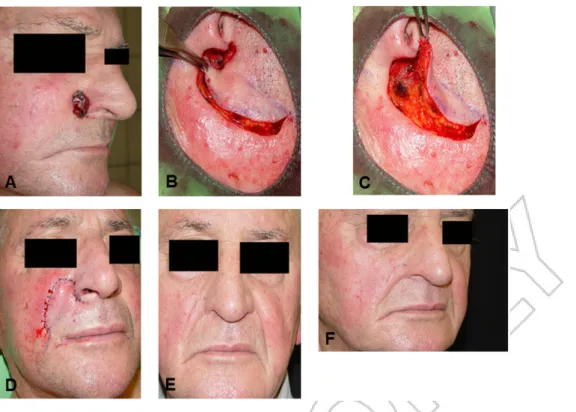
FIGURE 2 Reconstruction in another patient. A: preoperative status, B: preparation of the flap, C: positioning of the flap, D:
early postoperative status, E and F: late postoperative status.
asked to rate the pain on a 10-point scale: no pain (¼0), unbearable pain (¼10) while a 5-point Likert scale was suggested for the other questions: very
satisfied (¼5), relatively satisfied (¼4), fairly satis- fied (¼3), relatively dissatisfied (¼2), and very dis- satisfied (¼1).
345 346 347 348 349 350 351 352 353 354 355 356 357 358 359 360 361 362 363 364 365 366 367 368 369 370 371 372 373 374 375 376 377 378 379 380 381 382 383 384 385 386 387 388 389 390 391 392 393 394 395 396 397 398 399 400 401 402
403 404 405 406 407 408 409 410 411 412 413 414 415 416 417 418 419 420 421 422 423 424 425 426 427 428 429 430 431 432 433 434 435 436 437 438 439 440 441 442 443 444 445 446 447 448 449 450 451 452 453 454 455 456 457 458 459 460
FIGURE 4 A further patient with the combined flap. A: preoperative status, B: preparation of the flap, C: positioning of the flap, D: early postoperative status, E and F: late postoperative status.
FIGURE 3 Application of the combined flap in a third patient. A: preoperative status, B: dissection of the flap, C: positioning of the flap, white arrow: the subcutaneous part of the flap via which perforators enter the flap, black arrow: direction of the cutaneous branches from the medial part of the flap, D: early postoperative status, E and F: late postoperative status.
4 G. Mohoset al.
Journal of Investigative Surgery
Statistical Analysis
Data analysis was performed with SigmaStat for Windows (Jandel Scientific, Erkrath, Germany).
Friedman repeated measures analysis of variance on ranks was applied for the evaluation of the data obtained from laser Doppler flowmetry. Time- dependent differences from the baseline were assessed by Dunn’s method. In Figure 5, median values (M) with the 25th and 75th percentiles (25p and 75p, respectively) are given, p<.05 was consid- ered statistically significant. Scores describing the complications and patient satisfaction are presented as mean values (m) and standard deviation (SD).
RESULTS
The authors performed a combined cutaneous and subcutaneous pedicled rotation-advancement skin flap, contrary to the widely applied subcutaneous island pedicle flap. With this method, there is no (or short) incision in the nasolabial fold. This preserves the vascular supply better and provides more pref- erable cosmetic results with fewer scars.
As concerns perfusion of the flaps, laser Doppler flowmetry has revealed a significant decrease in the blood flow after preparation of the flap (M¼36.57 P.U., 25p¼22.02, 75p¼58.03) and fixation of the flap (M¼49.49 P.U., 25p¼29.1, 75p¼77.99) as compared to the baseline (M¼237.59 P.U., 25p¼152.89, 75p¼331.2). However, microcirculation has shown a considerable improvement during the 1st postopera- tive day. Day 1 perfusion values (M¼200.32 P.U., 25p¼106.34, 75p¼260.59) did not differ significantly from baseline. Sufficient blood flow was observed in the later period, as well. Week 3 values (M¼173.39 P.U., 25p¼132.59, 75p¼222.94) did not display sig- nificant difference as compared to the baseline (Figure 5).
Mild edema was noticeable in three cases during the 2nd-8th postoperative weeks (score: m¼0.3; SD
¼0.48) that was resolved with scar treatment and massage of the flap. In two cases, mild erythema was observed (score: m¼0.2; SD ¼0.42) which
ceased after the antibiotic therapy. Mild trap-door deformity was found in one case (score: m¼0.1; SD
¼0.32). Hematoma was not observed and none of the patients required reoperation/resuturing (Table 1).
The 6-month postoperative cosmetic result was out- standing. There were no further complications or need for additional correction (Figures 1F, 2E, 2F, 3E, 3F, 4E,4F).
Table 2 summarizes the findings of the patient satisfaction survey. The majority of the patients reported only mild or moderate postoperative pain.
They were also satisfied with the esthetic and the functional results of the intervention. Moreover, they have received positive feedback from other people.
DISCUSSION
The reconstruction of nasal soft tissue defects local- ized to multiple esthetic subunits is a challenging task for plastic surgeons. The combined reconstruc- tion of alar and perialar regions is difficult. The alar region has a rigid structure and low mobility, while the perialar soft tissues are different. Preserving the natural alar contours and concavities of the alar crease also keeping the respiratory function and symmetry with the contralateral side is important [2]. There are various reconstructive techniques available that can be used in this region, including direct closure, skin grafts, local flaps, regional pedicled flaps or combinations of these [7]. Direct closure is only preferable in case of small defects, because it can easily cause alar rim distortion. Skin grafts may result in depressed scars and impaired nasal valve patency when used to repair deeper alar 462
463 464 465 466 467 468 469 470 471 472 473 474 475 476 477 478 479 480 481 482 483 484 485 486 487 488 489 490 491 492 493 494 495 496 497 498 499 500 501 502 503 504 505 506 507 508 509 510 511 512 513 514 515 516 517 518
520 521 522 523 524 525 526 527 528 529 530 531 532 533 534 535 536 537 538 539 540 541 542 543 544 545 546 547 548 549 550 551 552 553 554 555 556 557 558 559 560 561 562 563 564 565 566 567 568 569 570 571 572 573 574 575 576
FIGURE 5 The blood flow of the flaps before the operation, during the intervention and in the postoperative period. Prep.
of the flap: preparation of the flap, Fix. of the flap: fixation of the flap. Median values with 25th and 75th percentiles are demonstrated. X:p<.05 vs. Baseline.
complications
Sign
Severity of the sign Mild Moderate Severe
Edema 3 0 0
Erythema 2 0 0
Hematoma 0 0 0
Trap-door deformity 1 0 0
Need for reoperation/resuturing 0
Number of patients displaying the given sign is presented.
defects [8]. Almost all local and regional flaps have significant drawbacks. The single staged nasolabial transposition flap results in a deformed alar groove thus producing an obvious asymmetry with the contralateral side [7]. The conventional subcutane- ous pedicled island flaps may also lead to distortion and more frequently pin-cushioning or trapdoor effect due to the all-round incision of the flap [4,9].
The combination of these procedures or multiple correctional surgeries can also be laborious and costly.
Our aim was to find a one-step intervention which fulfills all the above mentioned requirements with the least complications. The blood supply of our flap is dual. It can be considered as the combin- ation of the unipedicle melolabial advancement flap and the melolabial island advancement flap described by Baker [10]. Contrary to the above men- tioned ones, our flap receives blood supply from two different directions. On the one part, cutaneous vessels enter the flap from the area of the nasolabial fold (because the flap is not incised medially).
Furthermore, the flap is not undermined (except the cranial part) therefore it has subcutaneous perfora- tors, as well.
For the better mobilization, cutback can be per- formed hereby making a hatchet flap, however it is not necessary in most cases. This technique allows the reconstruction of alar and perialar defects local- ized to more esthetic subunits. As concerns prepar- ation of the flap, two different movements shall be performed. The flap is first moved to the inferior part of alar rim like an advancement flap. This is the pivot point around which the cranially thinned flap is rotated into the remaining part of the defect.
Regarding the results of the follow-up, there were no partial or complete flap losses. This may originate in the above mentioned advantageous blood supply which involves both cutaneous branches and subcutaneous perforators. Although surgical intervention itself may lead to a decrease in
capillary flow during the early postoperative period, this parameter shows regeneration then [11]. Neither hematoma, nor recurrence of the tumor was observ- able. Although in two cases sign of infection was detected, this may originate in the age and the comorbidities of the patients. Symmetry with the opposite side remained intact with no significant distortion or disfiguring of facial folds or creases.
Large defects may be accompanied with the risk of temporary or permanent distortion of upper lip and melolabial fold. The biggest defect in our study was 2.62.9 cm which has not led to such problem.
However, each case shall be judged individually, and our elderly patients possess a skin laxity which may facilitate the procedure. However, a slight edema of the flap was seen in some cases but this resolved with scar treatment and massage of the flap by the end of the 8th postoperative week. Mild trap-door deformity was found in one case and there was no need for a second operation in any of the cases. Furthermore, the patients were satisfied with the results of the intervention.
Planning of the flap is easy and with cautious dissection and trimming of the cranial part of the flap, the vascular supply can be fully preserved.
Our study involves mainly elderly patients since extended basal cell carcinoma is rare in younger patients. Elder skin may differ from that of younger patients in terms of laxity and microcirculation. Lax skin may facilitate positioning of the flap.
Microcirculation often displays impairment with the age, but we have found good postoperative regener- ation of blood flow and optimal flap survival.
Nevertheless, our future aim is to increase the num- ber of cases in order to gain more reliable data on this technique.
In conclusion, our flap design provides the ben- efits of the combined vascular supply of subcutane- ous and cutaneous pedicled flaps without the disadvantages of all-round incisions causing trap- door deformities. It is suitable for the reconstruction 577
578 579 580 581 582 583 584 585 586 587 588 589 590 591 592 593 594 595 596 597 598 599 600 601 602 603 604 605 606 607 608 609 610 611 612 613 614 615 616 617 618 619 620 621 622 623 624 625 626 627 628 629 630 631 632 633 634
635 636 637 638 639 640 641 642 643 644 645 646 647 648 649 650 651 652 653 654 655 656 657 658 659 660 661 662 663 664 665 666 667 668 669 670 671 672 673 674 675 676 677 678 679 680 681 682 683 684 685 686 687 688 689 690 691 692
TABLE 2 Patient satisfaction
Question Score
Q1: Could you rate the pain you felt after the intervention on a scale 0-10? m¼3.25; SD¼3.4 Q2: Are you satisfied with the esthetic result of the intervention? m¼4.5; SD¼0.58 Q3: Are you satisfied with the functional result of the intervention? m¼4.75; SD¼0.5 Q4: Are you satisfied with the feedback of other people (relatives,
acquaintances, etc.) concerning the result of the intervention?
m¼5.0; SD¼0 Q5: Are you satisfied with the present shape of your nose? m¼4.75; SD¼0.5 Q6: Are you satisfied with the healing of the wound and the scar? m¼4.5; SD¼0.58 Q7: Do you find the breathing through your nose satisfactory? m¼5.0; SD¼0 Q8: Would you decide to undergo this intervention for reconstruction,
if a facial tumor was removed again?
m¼4.75; SD¼0.5
For question 1, the answer was given on a scale 0-10, no pain (¼0), unbearable pain (¼10). concerning questions 2-8, a 5-point likert scale was applied: very satisfied (¼5), relatively satisfied (¼4), fairly satisfied (¼3), relatively dissatisfied (¼2) and very dissatisfied (¼1). m: mean value, SD: standard deviation.
6 G. Mohoset al.
Journal of Investigative Surgery
appropriate cosmetic result.
DECLARATION OF INTEREST
The authors report no conflict of interest. The authors are alone responsible for the content and writing of the paper.
REFERENCES
[1] Cvancara JL, Wentzell JM. Shark island pedicle flap for repair of combined nasal ala-perialar defects. Dermatol Surg.2006;32(5):726–729.
[2] Padoveze EH, Cernea SS. Reconstruction of nasal defects after tumor excision through Mohs micrographic sur- gery.Surg Cosmet Dermatol.2013;5(2):116–120.
[3] Levasseur JG, Mellette JR, Jr. Techniques for reconstruc- tion of perialar and perialar-nasal ala combined defects.
Dermatol Surg.2000;26(11):1019–1023.
[4] Li JH, Xing X, Liu HY, Li P, Xu J. Subcutaneous island pedicle flap: variations and versatility for facial recon- struction. Ann Plast Surg. 2006;57(3):255–259. doi:
10.1097/01.sap.0000221639.76906.3a
ment and clinical application. Iowa Orthop J. 1991;11:
119–126.
[6] Varga J, Mohos G, Varga A, et al. A possible technique for the complex reconstruction of exposed breast implant: applicability and microcirculation of the capsule flap.J Invest Surg.2018:1. doi:10.1080/08941939.2018 Q1
[7] Tregaskiss A, Allan J, Gore S, Aldred R. Use of nasal sidewall island inversion flap for single-stage ala nasi reconstruction: a report of 103 consecutive cages. Plast Reconstr Surg. 2014;133(2):377–385. doi:10.1097/
01.prs.0000436797.81928.24
[8] Pipitone MA, Gloster HM. Jr., Repair of the alar groove with combination partial primary closure and second- intention healing.Dermatol Surg.2005;31(5):608–609.
[9] Szolnoky G, Mohos G, Dobozy A, Kemeny L. Manual lymph drainage reduces trapdoor effect in subcutaneous island pedicle flaps. Int J Dermatol. 2006; 45(12):
1468–1470. doi:10.1111/j.1365-4632.2006.03165.x
[10] Baker SR. Melolabial flaps. In: Baker SR (ed). Local flaps in facial reconstruction. 2nd ed. Edinburgh: Elsevier Mosby;2007: 231–264.
[11] Figus A, Mosahebi A, Ramakrishnan V. Microcirculation in DIEP flaps: a study of the haemodynamics using laser Doppler flowmetry and lightguide reflectance spectro- photometry. J Plast Reconstr Aesthet Surg. 2006; 59(6):
604–612.
694 695 696 697 698 699 700 701 702 703 704 705 706 707 708 709 710 711 712 713 714 715 716 717 718 719 720 721 722 723 724 725 726 727 728 729 730 731 732 733 734 735 736 737 738 739 740 741 742 743 744 745 746 747 748 749 750
752 753 754 755 756 757 758 759 760 761 762 763 764 765 766 767 768 769 770 771 772 773 774 775 776 777 778 779 780 781 782 783 784 785 786 787 788 789 790 791 792 793 794 795 796 797 798 799 800 801 802 803 804 805 806 807 808